Wishing you a Happy Thanksgiving Day
Iris Publishers Journal of Nutrition And Food Science
Iris Publishers Journal of Nutrition & Food Science is an interdisciplinary journal that offers accessible and comprehensive coverage of research that undergoes in food world. Our aim is to bring awareness in people regarding how our food style affects the daily routine and measures to be taken to avoid the complications and diseases which occur due to unbalanced diet. Hence, we are creating a platform to the research lovers to produce their works to the world
Wednesday, 24 November 2021
Tuesday, 22 June 2021
Iris publishers-Global Journal of Nutrition & Food Science (GJNFS)
Methanol Leaf Extract of Diospyros Chloroxylon Attenuates Chlorpyrifos-Induced Toxicity in Rats
Abstract
Background and Objective: Chlorpyrifos [O, O-diethyl-O-(3, 5, 6-trichloro-2-pyridyl)-phosphorothioate] (CPF) is a broad-spectrum Organophosphate insecticide that are used in many farms and homes. Despite the several reported toxicity in humans, there has been virtually no alternative effective insecticide. Thus, the amelioration of the toxicities seems the best option in alternative medicine. This study, therefore, investigated the effects of methanol extract of Diospyros chloroxylon leaf (MEDCL) on the brain and heart of rats exposed to CPF.
Materials and Methods: Twenty-four rats were randomized into four groups of 6 rats each, and treated separately with distilled water (Control), CPF (5 mg/kg), MEDCL (100 mg/kg) and MEDCL (100 mg/kg) + CPF (5 mg/kg), following 7 days of acclimatization. After 4 weeks of treatments, the rats were sacrificed, and the levels of Superoxide dismutase (SOD), Catalase (CAT), Malondialdehyde (MDA), reduced glutathione (GSH), Glutathione peroxidase (GPx), glutathione S-transferase (GST) and DNA fragmentation were spectrophotometrically assessed in the brain and heart, while Acetylcholinesterase (AChE) activities were assessed in the serum and brain of the rats.
Results: The results showed that CPF significantly reduced the levels of SOD, CAT, GSH, GPx and GST, while that of MDA was elevated in brain and heart, compared with controls. Treatment with CPF significantly lowered the activities of AChE in serum and brain by 94% and 48% respectively, while the level of DNA fragmentation was significantly elevated in the CPF-treated rats. Supplementation with MEDCL significantly ameliorated the changes in the rats.
Conclusion: From the foregoing, the suppressive potential of methanol extract of Diospyros chloroxylon leaf is marked indicated in brain and cardiac redox imbalance induced on exposure to Chlorpyrifos.
Keyword: Chlorpyrifos; Diospyros chloroxylon; Oxidative stress; Acetylcholinesterase; DNA fragmentation
Introduction
Chlorpyrifos [O, O-diethyl-O-(3,5,6-trichloro-2-pyridyl)- phosphorothioate] (CPF) is an organophosphate insecticide, acaricide and miticide used in protection of various crops and ornamental plants [1]. Chlorpyrifos becomes introduced into the environment via direct application on crops, lawns, domesticated animals, as well as in homes and workplaces. However, volatilization is the major way in which this organophosphate is dispersed in the environment, after application. In the environment, it becomes decomposed through the sunlight, bacterial and chemical processes [2]. Mackay, et al. [3] has observed the atmospheric formation of Chlorpyrifos oxon from Chlorpyrifos. The hepatic biotransformation of Chlorpyrifos has been reported to involve cytochrome P-450 dependent desulfuration, to form Chlorpyrifos oxon [4,5]. This oxon is rapidly hydrolyzed to 3, 5, 6-trichloro-2-pyridinol (TCP) through the activity of Aryl- esterase. Both bioactivation and detoxification of Chlorpyrifos have been suggested to occur very rapidly, since TCP was detected as the only metabolite in the hepatic effluent under steady-state conditions 4. The TCP has been noted to be, in several orders of magnitude, less toxic than either Chlorpyrifos or its oxon form [6,7].
Some earlier studies by Bakke, et al. [8] and Nolan, et al. [9] had indicated that the hydrolysis of Chlorpyrifos oxon by A-esterase could probably be a common route of detoxification, since TCP or its conjugate is the major metabolite detected in rodents and humans. A kinetic study of the relative rates of deulfuration and detoxification of Chlorpyrifos by Chambers and Chambers [10] suggested a gender-dependence, which may explain its higher toxicity in female rats than male ones. Various mutagenicity studies using Chorpyrifos revealed that it could cause metaphasic chromosomal aberrations in mouse spleen cell culture [11], sister chromatid exchange in human lymphoid cells [12] and induction of micronuclei, chromosomal lesions, and DNA damage in many organisms [13-15]. However, the USEPA [16] reported the nonmutagenicity of Chlorpyrifos in both bacterial and mammalian cells but did noticed slight genetic aberrations in yeast and DNA in bacterial cells. Tumor developments in mammalian organs, such as prostate [17], breast [18,19] and rectum [20] have been reported to be caused by Chlorpyrifos exposure.
The hepatic cytochrome P-450 dependent metabolism of testosterone and estradiol has been noticed to be inhibited Chlorpyrifos exposure [21,22]. Furthermore, this organophosphate insecticide has been reported to cause decrease in testicular testosterone biosynthesis, and low productions of major steroidogenic enzymes, steroidogenic acute regulatory (StAR) protein and luteinizing hormone receptor stimulated cAMP as investigated by Viswanath, et al. [23].
Diospyros choloroxylon is a widely distributed shrub, belonging to the Diospyros species of the family, Ebenaceae [24]. This shrub and some other members of the species have been used in orthodox medicine all over the world in treatments of several ailments and diseases [25-27]. Studies have shown a possible link between the medicinal potential of D. chloroxylon and the presence of secondary metabolites, such as, alkaloids, flavonoids, tannins, saponins, triterpenoids and phenolics [28]. An important triterpenoid, betulinc acid, present in Diospyros species [29], has been reported to possess several biological properties [30-35]. In the recent time, methanol extract of D. chloroxylon leaf has been reported potent against some environmental toxicants [36,37]. In the present study, the hypothesis was that methanol extract of Diospyros chloroxylon leaf could attenuate redox-induced injuries in the brain and heart of rats exposed to Chlorpyrifos.
Materials and Methods
Duration and place of study
Both experimental work and data analysis were carried out between the months of February and June 2018, in the Department of Biochemistry, Ladoke Akintola University of Technology, Ogbomoso, Oyo State, Nigeria.
Chemicals
Glutathione, Epinephrine, 5, 5 dithiobis-(2-nitrobenzoate) (DTNB) and hydrogen peroxide were purchased from the Sigma chemical Co. Saint Louis, MO, USA. Trichloroacetic acid, 2-thiobarbituric acid, Triton X-100 and Diphenylamine were purchased from the British Drug House (BDH) Chemical td, Poole, U.K. All other reagents were of good analytical grades.
Collection and extraction of Plant material
The leaves of Diospyros chloroxylon were bought in February 2018, from a local herb seller in Ogbomoso, and authenticated at the Department of Biology, Botany Unit, Ladoke Akintola University of Technology, Ogbomoso, Oyo State, Nigeria. The leaves were washed with distilled water, air-dried, and pulverized with an electrical grinder. The leaf powder was soaked in methanol for 72 hours. The extraction was repeated twice, and the extract was collected, filtered, and concentrated under vacuum using rotary evaporator at 45oC. The resulting crude extract was stored under refrigeration at 4oC.
Experimental animals and design
Twenty-four (24) male Wistar rats (140.09±9.61 g) were bought from the Animal house of the Institute for Advanced Medical Research and Training (IAMRAT), University of Ibadan, Nigeria. The rats were later brought to the Animal house of the Department of Biochemistry, Ladoke Akintola University of Technology, Ogbomoso, Oyo State, Nigeria. They were randomized into four (4) groups (6 rats each) and housed in plastic cages and fed on rat pellets and drinking water (ad libitum) for 7 days of acclimatization, under 12-h light/dark cycle and temperature of 29±2oC. The 4 groups of rats were separately treated as follows: distilled water (Control), CPF (5 mg/kg), methanol extract of D. chloroxylon leaf (MEDCL) (100 mg/kg), and CPF (5 mg/kg) + MEDCL (100mg/kg). CPF and MEDCL were administered twice per week and every other day, respectively for 4 weeks.
Collection of blood and organs
After 4 weeks, the rats were fasted overnight. Blood was collected into non-heparinized bottles by ocular bleeding and animals were sacrificed by cervical dislocation. Blood was allowed to clot and then centrifuged at 3000xg for 10 minutes to obtain serum. Brain and heart were excised, washed in ice-cold 1.15% potassium chloride solution to remove blood stains. Each organ was divided into 2 portions, one portion was homogenized with phosphate buffer (pH 7.4) using a Teflon homogenizer and centrifuged using a high speed refrigerated centrifuge (HITACHI) at 10,000xg for 10 minutes to obtain homogenate used for antioxidant and Acetylcholinesterase assays. The other portion of organs was kept for DNA fragmentation assay.
Biochemical assays
Determination of protein level: Protein levels of brain, heart and serum were determined as described by Lowry, et al. [38] using Bovine serum albumin as the standard.
Determination of malondialdehyde level: Malondialdehyde (MDA) levels of brain and heart were estimated as described by Ohkawa, et al. [39]. The absorbance of the clear pink supernatant was measured spectrophotometrically against a reference blank at 532 nm. The MDA concentration was calculated using a molar extinction coefficient (Ɛ) of 1.56 x 105 M-1cm-1.
Determination of superoxide dismutase activity: Superoxide dismutase activities of brain and heart were measured by the epinephrine method described by Misra and Fridovich [40]. The increase in absorbance of the assay reaction at 480 nm was monitored spectrophotometrically at 30 seconds intervals for 150 seconds. The specific activity of SOD was expressed in units/mg protein.
Determination of catalase activity: Catalase activities of brain and heart were assayed according to the method of Aebi [41]. The method is based on the ability of catalase to promote decomposition of hydrogen peroxide in a reaction mixture. The change in absorbance 240 nm was monitored spectrophotometrically at 60 seconds intervals for 180 seconds. Catalase activity was expressed as units/mg protein.
Determination of glutathione peroxidase activity: Glutathione peroxidase (GPx) activities of brain and heart were determined using the method described by Andersen, et al. [42]. The assay is based on the reaction of organic peroxide in a reaction mixture and oxidation of reduced glutathione (GSH) to form disulfide glutathione (GSSG). The GSSG is later reduced to GSH by glutathione reductase and NADPH. The decrease in absorbance at 412 nm is directly proportional to the GPx activity, which is expressed in μmol/mg protein/min.
Determination of reduced glutathione level: Reduced Glutathione (GSH) levels of brain and heart were determined using the method of Mitchell, et al. [43]. The assay is based on the oxidation of GSH by sulfhydryl reagent DTNB, to form a yellow derivative, 51-thio-2-nitrobenzoic acid, with an absorbance at 412 nm. GSH level is proportional to absorbance at 412 nm. Values were expressed as U/ mg protein.
Determination of glutathione-s-transferase activity: Glutathione-S-transferase (GST) activities of brain and heart were assayed according to the method of Habig, et al. [44]. The method is based on the ability of GST to catalyse the conjugation of L-glutathione and CDNB to form a conjugate, GS-DNB, with an absorbance at 340 nm. The rate of increase in absorbance at 340 nm is directly proportional to GST activity. Specific activities were expressed as μM/mg protein/min.
Determination of acetylcholinesterase activity: Acetylcholinesterase (AChE) activities of serum and brain were determined using the method described by Ellman, et al. [45], with acetylthiocholine iodide as a substrate. In this method AChE hydrolyzes acetylthiocholine iodide into thiocholine and butyric acid. The thiocholine reacts with 5, 5-dithiobis-2- nitrobenzoic acid (DTNB) to form 5-thio-2-nitrobenzoic acid to form a yellow product whose absorbance is measured spectrophotometrically at 412 nm.
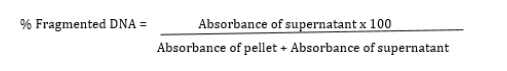
Determination of DNA fragmentation level: Finally, a spectrophotometric method described by Wu et al.46 was used to determine the percentage fragmented DNA. Briefly, the brain and heart were homogenized in Tris-HCl-EDTA (lysis) buffer and centrifuged at 27,000 x g for 10 mins to separate the intact DNA (pellet) from the fragmented DNA (supernatant). Both the pellet and supernatant were treated with freshly prepared DPA reagent for colour development. The mixtures were incubated at 370C for 20-24 hours. The absorbance was read spectrophotometrically at 620 nm. The percentage fragmented DNA was calculated using the formula:
Statistical Analysis
All values were expressed as the mean±standard deviation of six rats per group. Data were analysed using the Graph Pad Prism 6.0 package. Level of significance among the groups was evaluated using one-way analysis of variance (ANOVA) followed by Tukey multiple comparison test. P values of < 0.05 were considered significant.
Results
Effect of MEDCL on body weight of CPF-exposed rats
The effects of Chlorpyrifos (CPF) on the body weights of the rats are presented in Table 1. Treatment with CPF significantly (p<0.05) reduced the body weight gain (in grammes) of the rats (10.26±1.9) relative to the control (35.97±2.7). In the MEDCL-supplemented rats, the weight gain was significantly increased (27.20±2.6 g) compared with the CPF-treated group.
Effects of MEDCL on oxidant parameters of CPF-exposed rats
The data in Table 2 show that CPF significantly (p < 0.05) reduced the activity of SOD (2.30±1.3 and 1.85±0.6 U/mg protein) versus control (5.14±1.2 and 3.54±1.0) in both brain and heart, respectively. Furthermore, the catalase activities were reduced (3.91±1.2 and 3.38±1.0 U/mg protein) versus control (6.88±1.5 and 3.93±0.4 U/mg protein) in brain and heart, respectively. Interestingly, supplementation with MEDCL significantly elevated the activities of SOD (4.68±1.6 and 3.14±0.6 U/mg protein) and Catalase (7.13±0.8 and 4.13±0.4 U/mg protein) in brain and heart, respectively relative to the CPF group.
The present study also examined the effects of the treatments on levels of lipid peroxidation (MDA) and reduced glutathione (GSH), as well as the activities of glutathione peroxidase (GPx) and glutathione S-transferase (GST) in the rats. Treatment with CPF caused the level of MDA to significantly (p<0.05) increase (6.51±1.0 and 1.25±0.3 μM MDA/ mg protein) in the brain and heart, respectively compared with control treatment (3.48±0.4 and 0.66±0.1 μM MDA/ mg protein). On supplementation with MEDCL, significantly lower levels of MDA were found as 2.95±0.7 and 0.75±0.2 μM MDA/ mg protein) in brain and heart, respectively compared with the CPF-treated rats (Figure 1).
The level of GSH was significantly (p<0.05) reduced by CPF administration in both brain (11.62±03 U/mg protein) and heart (9.74±10U/mg protein) as against the controls (18.77±14 and 15.56±12 U/mg protein), respectively. When MEDCL was administered, the levels were elevated, and found to be 17.51±3.2 and 15.91±1.8 U/mg protein, in brain and heart, respectively compared with the CPF group, as shown in (Figure 2).
Table 3 presents the results on GPx and GST activities during the treatments. Chlorpyrifos was observed to significantly (p < 0.05) reduce GPx activity in brain (6.74±1.0 U/mg protein) and heart (2.13±0.5 U/mg protein) relative to the respective controls (8.47±2.1 and 3.48±1.2 U/mg protein). However, supplementation with MEDCL significantly attenuated the CPF- induced effects in the two organs, as shown in Table 3. Furthermore, CPF was found to significantly (p < 0.05) reduce GST activities in the brain (2.75± 0.8μM/mg protein) and heart (1.13±0.2μM/mg protein) compared with the control rats (5.04±1.2 and 2.48±0.9μM/mg protein, respectively) as shown in table 3. On supplementation with MEDCL, the activities were found to be 4.05±1.4 and 2.98±0.8 μM/ mg protein in the respective organs compared with the CPF-treated rats.
Effects of MEDCL on Acetylcholinesterase activity and DNA fragmentation in CPF-exposed rats
The result in Figure 3 shows that CPF treatment caused the AChE activities to significantly (p < 0.05) decrease in brain (0.11±0.0 U/ml) and heart (0.18±0.1 U/ml), when compared with the control treatment (0.19±0.1 and 0.25±0.0 U/ml). When supplemented with MEDCL, the activities of AChE enzyme were observed to be 0.21± 0.1 U/ml (brain) and 0.24±0.0 U/ml (heart) in the experimental rats. The result of the effect of CPF on the percentage of DNA fragmentation in the two organs has been presented in (Figure 4).
Treatment with CPF significantly (p<0.05) elevated the level of fragmented DNA in brain (49.51±2.4 %) and heart (64.78±5.3 %), compared with the controls (28.47±3.1 and 32.50±3.8 %, respectively). Interestingly, supplementation with MEDCL significantly attenuated the CPF-induced DNA damage in brain (30.90±3.2 %) and heart (44.20±5.1 %) in the rats.
Discussion
The major findings in the present study include induction of oxidative stress, DNA damage and inhibition of Acetylcholinesterase activity in rats exposed to Chlorpyrifos. Interestingly, these adverse changes were attenuated on treatment of the experimental rats with methanol extract of Diospyros chloroxylon leaf (MEDCL).
The rats exposed to CPF were noticed with a significant reduction in body weight gain, while on supplementation with the extract, the effect was improved comparable to the control animals. Studies conducted by Perera, et al. [47] and Whyatt, et al. [48] found a correlation between CPF intoxication and reduced birth weight and body length. This reduction may be a result of loss of appetite, malabsorption, and digestive disorder, as reported by Neuget, et al. [49].
Oxidative stress results from the imbalance between the reactive oxygen species (ROS) and antioxidant defence system of the cells, causing oxidation of DNA, protein, or lipid molecules. The damage, in turn, may result in several events, such as, altered gene expression [50], enhanced cell proliferation [51], genomic or chromosome instability, genetic mutation or tumour development [52,53].
The data from this study showed that SOD and catalase activities were significantly reduced in both brain and heart on exposure of the rats to CPF. Malondialdehyde (MDA) is a reactive aldehyde formed because of the reaction of ROS with polyunsaturated fatty acids [54]. The elevated level of MDA indicates an induction of lipid peroxidation, hence oxidative damage in the organs of the CPFtreated animals. The toxicant also significantly reduced the levels of GSH, GPx and GST in the two organs of the animals compared with the controls. In several tissues, including brain, liver, and testis, CPF has been demonstrated to cause increase in lipid peroxidation (MDA level) [55, 56] and decrease in catalase, SOD, GPx and GST [57-60]. According to Bebe and Panemangalore [61], low doses of CPF were demonstrated to cause decrease in GSH and increase in GPx, although the level of GSH was found to increase during treatment with higher CPF doses.
Catalase is an endogenous antioxidant enzyme capable of removing ROS via conversion of hydrogen peroxide to water and oxygen [62], while GPx are a group of seleno-proteins involved in cellular protection against oxidative damage induced by hydrogen peroxide and organic peroxides [63]. Reduced glutathione (GSH), on the other hand, serves as a substrate for glutathione peroxidase (GPX) during detoxification, by being oxidized to GSH disulfide (GSSG). The GSSG is converted back to which is converted back to GSH through the activity of glutathione reductase (GPR) [64]. Decrease in level of GSH has been associated with low availability of cysteine molecules required for GSH production, which in turn has resulted from defect in transulfuration characteristic of liver damage [64].
Glutathione-S-transferases (GSTs) belong to a major group of phase II detoxification enzymes, responsible for the conjugation of several endogenous and exogenous reactive electrophiles with GSH [65]. Inhibition of GST activity has been suggested by Binkova, et al. [66] as a mechanism of potentiating the toxicity of environmental chemicals, resulting in increased interactions between them (or their metabolites) and cellular macromolecules. In rats and mouse, CPF is bioactivated in the liver, through cytochrome-p450-dependent pathway, to form CPF-oxon [67,68], which is a more toxic metabolite. The observed reduction in the activities of the antioxidant enzymes in the present study may thus indicate the inhibitory influence of CPF-oxon, which has therefore enhanced accumulation of ROS, leading to oxidative imbalance in the two organs of the rats. This finding is supported by a study carried out by Ventura, et al. [19], who reported that Chlorpyrifos caused increase in the level of ROS in certain breast cancer cell lines. Furthermore, CPF has been demonstrated to induce oxidative stress in rat testes, leading to reductions in sperm count, systemic testosterone, gonadotropin levels and activities of enzymes catalysing spermatogenesis [69]. In the group of animals supplemented with MEDCL, the activities of the antioxidant enzymes were significantly improved, while the level of MDA was reduced relative to the toxicant group. In a recent study, betulinic acid, a triterpenoid reported to be present in Diospyros species [29], has been demonstrated to improve the activities of SOD, Catalase, GPx and GST, as well as the level of MDA in experimental rats treated with an environmental toxicant34. This thus suggests the potential of the Diospyros chloroxylon leaf extract used in this study to ameliorate the imbalance in antioxidant status of the rats.
The present study also examined the effects of CPF on the Acetylcholinesterase (AChE) activities in the brain and serum of the experimental animals. Significantly decreased activities of the enzyme were observed in rats treated with CPF relative to control rats. In several studies, CPF treatment was shown to cause neurological effects such as, sensory loss, memory impairment and depression in AChE activities in many animal species [70-72]. In a study by Cutler, et al. [73], it has been shown that CPF itself is not a potent inhibitor of AChE, but its metabolite, CPF-oxon. This metabolite phosphorylates the serine hydroxyl group at the active site of AChE enzyme, through a nucleophilic interaction, resulting in accumulation of acetylcholine, with subsequent neurotransmission disruption and death [74]. Some other studies have revealed that in the earliest stage of brain and central nervous system development, CPF mitigated neural formation, and caused reduction in the cholinergic projections [75]. This resulted in reduced neural connections, cell signalling capacity, and eventual deficiency in cholinergic synaptic response with behavioural problems in adolescence and adulthood [76]. However, CPF has been demonstrated to preferentially exert toxicity in brain glial cells, which are formed later than the neuronal cells [77,78]. Furthermore, this toxicant exerted adverse effects on the proliferation, differentiation and functioning of glial cells, as well as the cells involved in the neuronal metabolism and targeting within the CNS in rats, during prenatal and postnatal exposures [19,79]. In addition, Sandoval et al [80] have reported that CPF could induce generation of astroglial cells, using human neural stem cells (hNSCs) line, without affecting neuron formation. However, this study has demonstrated that supplementation with MEDCL against CPF treatment improved the activity of AChE enzyme in both brain and serum of the rats, indicating the potential of the extract in improving cholinergic transmission in the rats.
The genotoxic effect of CPF in the brain and heart of the rats was also examined by determining the level of DNA fragmentation as described by Wu, et al. [46]. The treatment with CPF caused a significant increase in DNA fragmentation compared with the controls. Interestingly, the ability of MEDCL to lower the amount of fragmented DNA against CPF treatment was observed. Various forms of genotoxic effect of CPF have been reported, including bone marrow micronuclei induction and DNA hypomethylation in mouse [15], chromosomal alterations, chromosomal breaks, and sister chromatid exchange in humans [81], and micronuclei induction and chromosomal lesions in erythrocytes [82]. The reduction in the level of DNA fragmentation by MEDCL, as observed in this study shows the potential of the extract to protect the organs from the DNA damaging effect of CPF. The overall findings have implied the potential of methanol extract of Diospyros chloroxylon leaf in ameliorating the toxic effects of chlorpyrifos in experimental rats. The study thus clearly shows the possible application of Diospyros chloroxylon leaf extract in the discovery of drugs against toxicity induced by environmental agents. It could therefore be recommended that Pharmaceutical Scientists could isolate, and work on, the active ingredients of Diospyros chloroxylon leaf, for the purpose of making a drug potent against oxidative and degenerative diseases. However, this study has some limitations in that only methanol was used for extraction, and the various compounds in the MEDCL were not elucidated.
Conclusion
The data from this study have shown that Chlorpyrifos (CPF) induced significant oxidative, neurotoxic and genotoxic damage in brain and heart of experimental rats. However, methanol extract of Diospyros chloroxylon leaf ameliorated the CPF-induced redox imbalance in the two organs of rats. Furthermore, the extract of Diospyros chloroxylon leaf exerted attenuation against the neurotoxic and DNA-damaging effects induced by chlorpyrifos in the experimental rats.
Significance Statement
This study discovered the potential of Diospyros chloroxylon leaf extract, which could be beneficial for treatments of oxidative and degenerative diseases induced by chlorpyrifos. This study will assist researchers towards the use of Diospyros chloroxylon leaf for drug discovery, which has not been previously explored. As a result, a new theory on treatments of oxidative and degenerative diseases, using Diospyros chloroxylon leaf may be put forth, in addition to the existing data on medicinal values of plants.
List of Abbreviations
CPF: Chlorpyrifos, MEDCL: Methanol extract of Diospyros chloroxylon leaf, SOD: Superoxide dismutase, CAT: Catalase, MDA: Malon-di-aldehyde, GSH: Reduced Glutathione, Gpx: Glutathione peroxidase, GST: Glutathione S-Transferase, AChE: Acetylcholinesterase, ROS: Reactive Oxygen Species
Ethical Approval and Consent to Participate
This study was carried out in accordance with ethical laws on animal handling.
Availability of Data and Materials
The dataset supporting the conclusions of this article are included as tables and figures in the within the article (and its additional files).
Authors Contributions
AGE conceived, designed and supervised the study. AOT cosupervised the study and read the final manuscript. AOO, AOE and BW provided the materials used in the study, collated literatures and performed the experimental procedures. EBO did the statistical analyses and drafted the manuscript. All authors financed of the study. All authors read and approved the final manuscript with the order of author’s names.
To read more about this article: https://irispublishers.com/gjnfs/fulltext/methanol-leaf-extract-of-diospyros-chloroxylon-attenuates-chlorpyrifos-induced-toxicity-in-rats.ID.000565.php
For more Open Access Journals in Iris publishers please click on: https://irispublishers.com/pdf/peer-review-process-iris-publishers.pdf
Tuesday, 15 June 2021
Iris publishers-Global Journal of Nutrition & Food Science (GJNFS)
Obesity Paradox in Kidney Diseases
Authored by Cagla Pinarli*
Abstract
Obesity is one of the most important health problem in the world. Elevated mortality risk can be seen with obesity, diabetes, hypertension, glomerular hyperfiltration, chronic kidney disease, and cardiovascular diseases. However, it has been observed that obesity positively affects survival especially in people with chronic kidney disease, elderly people, chronic heart failure, chronic obstructive pulmonary disease, cancer, acquired immune deficiency syndrome and rheumatoid arthritis. This situation has been called the obesity paradox. Studies are showing that the obesity paradox is valid in dialysis patients. Examinations have shown that the obesity paradox is affected by many factors such as ethnic origin, fat-muscle mass, and body mass index (BMI). The hypothetical pathophysiology of the obesity paradox reveals how obesity improves survival in chronic kidney disease.
Keyword: Obesity paradox; Obesity; Kidney diseases
Abbreviations: BMI: Body Mass Index, CKD: Chronic Kidney Disease, ESRD: End-Stage Renal Disease
Introduction
People with chronic kidney disease (CKD) have an increased mortality rate with end-stage renal disease (ESRD) and dialysis treatment. Mortality reaches up higher in the first months of dialysis therapy [1]. The mortality level seen in patients with chronic kidney disease is even higher than the risk of death seen in many types of cancer [2]. According to the results of randomized clinical studies, no significant benefit was found between improvement in CKD-related specific factors (anemia, iron deficiency, hyperphosphatemia, hyperparathyroidism, vitamin D deficiency, hypercalcemia, and dialysis dose) and survival [3,4]. At this point, it has been observed that the obesity paradox has a significant relationship with survival [5,6].
Obesity and CKD
Studies show that obesity, in general, has an accelerating effect on the risk of CKD [7]. According to the results of a study, it is thought that weight loss may have an anti-CKD effect. As a consequence of some bariatric surgery operations, a reduction in EGFR has been observed. It has been stated that this situation can prevent glomerular hyperfiltration and decrease the risk of CKD [8]. On the other hand, if CKD occurs, increased BMI is paradoxically related to survival [9].
Hypothetical Pathophysiology of the Obesity Paradox
The pathophysiology of protein-energy deficiency in CKD occurs with inflammation. Thus, inflammatory cytokines (interleukin-6, tumor necrosis factor-α) repress appetite, cause hypoalbuminemia and muscle destruction. By the loss of muscle and fat mass, inflammation, increased cardiovascular disease, and death result. Obesity has a potential protective effect against protein-energy deficiency. Obesity defends against inflammation and reduces the risk of cardiovascular disease and death. For example, patients with excess adipose tissue are at a lower risk for protein-energy deficiency because they have more energy and protein reserves. Therefore, a lower risk of death is observed in dialysis patients with high BMI or creatine concentration [10,11]. On the other hand, obesity is related to short-term hemodynamic stability. Fluid accumulation and heart failure are seen in many CKD patients on dialysis. In contrast to similar pulmonary capillary occlusion pressure, increased systolic blood pressure is seen in obese and overweight subjects. This provides better tolerance to the ultrafiltration rate and high volume occurring during dialysis [12]. The change in cytokines provides better results in obese individuals. Adipose tissue produces tumor necrosis factor-α receptor. Increased number of receptors play a cardioprotective role. Body fat and weight loss boost the release of lipophilic hexachlorobenzene and other chlorinated hydrocarbons. This demonstrates the enhanced risk of mortality in ESRD patients. Obese cases have an increased lipid and lipoprotein combination. This can calm the circulating endotoxins. Eventually, cardiovascular diseases and death occur [13,14]. Importantly, it should be emphasized that enhanced BMI level due to increased muscle mass was found to be more effective in the obesity paradox (compared to fat mass) [15].
Ethnicity and Obesity Paradox
There are also studies showing how ethnicity affects the obesity paradox. The obesity paradox was found to be stronger in African Americans in a study conducted on dialysis patients [16]. In another study, the stronger relationship was observed between elevated BMI and survival in African Americans, Asian Americans, Caucasians and Hispanics [17].
Conclusion
Obesity paradox is common in chronic diseases, especially in conditions such as advanced CKD, where weight loss is common. Studies show that obesity, in general, has an increasing effect on the risk of CKD disease, but on the other hand, if CKD occurs, the increased BMI is paradoxically associated with survival. It has been observed that weight loss leads to an increased risk of death in dialysis patients. Weight loss, primarily in the earliest months, is linked to increased mortality. An improvement in fat and muscle mass is generally associated with improved survival in people with CKD. The increase in muscle mass has an extra protective effect. Studies on the relationship between ethnicity and the obesity paradox show that the obesity paradox is observed in some ethnicity more powerfully.
To read more about this article: https://irispublishers.com/gjnfs/fulltext/obesity-paradox-in-kidney-diseases.ID.000564.php
For more Open Access Journals in Iris publishers please click on: https://irispublishers.com/pdf/peer-review-process-iris-publishers.pdf
Wednesday, 9 June 2021
Iris publishers-Global Journal of Nutrition & Food Science (GJNFS)
Covid-19 Vaccination Side Effects and Foods That Can Help
Introduction
The year 2020 was awash with Covid-19 (also known as the corona virus) contraction numbers, details, and death tolls. As a country, we are now moving into a new stage as more people receive the Covid-19 vaccine. There have been lots of myths and fallacies regarding the vaccine such as “when a person gets vaccinated a microchip is implanted with spying capabilities” or “the vaccine will give you the virus.” I am happy to say that none of these urban legends are true. However, with all the talk about Covid-19 vaccines and how one will feel afterward, focusing on foods that sooth the body and make you feel better after being vaccinated is a positive, proactive way to help your body recover and perhaps ease your mind just a little. Food does not just nourish the soul; it also has many healing properties that can give your body a boost and may help to prevent and manage some symptoms [1].
Effects of Covid-19 Vaccinations
First, let us try to understand the Covid-19 vaccine a little more. According to Dr. Marlene Millen, Chief Medical Information Officer, Ambulatory & Primary Care Physician at UC San Diego Health, the vaccine cannot cause contraction of Covid-19, no more than the flu vaccine can give you the flu. Your first Covid-19 vaccination will likely cause you to have soreness in the vaccination area, perhaps a low-grade fever or chills. Acetaminophen (Tylenol©) is a sufficient pain reliever and will cause one to feel better overall. Dr. Millin suggests that these symptoms will last approximately 24-48 hours [2].
The Center for Disease Control and Prevention states that the second round of the Covid-19 vaccine has aftereffects that are somewhat stronger. They stated that “people who get the second dose of the COVID-19 vaccine experience more frequent and severe side effects as opposed to when they receive the first dose. That includes sometimes headache, sometimes fever or even body malaise or kind of fatigue [3].” The CDC also made clear that younger people are more impacted by the side effects after the second dose than older people are [3].
Dr. Emmanuel Sarmiento, MD is an Allergy & Immunology Specialist in Greenville, SC. He explained that you “should not do any strenuous activities, stay rested, hydrate and take your Tylenol.” He also stated that “the first dose is given to have the body build up the immune response, while the second dose is given to boost that response.” This means that your body is reacting and the symptoms you are experiencing are in response to the vaccine. Dr. Sarmiento also stated that “you may have more symptoms from the second dose because that’s when you are producing a lot of antibodies.” He also states that while the first 30 minutes after the shot is when most severe allergic reactions could take place, he also adds that while temporary and manageable, the other side effects could last for 24-48 hours [4].
Dr. Greg Poland, Director of the Mayo Clinic’s Vaccine Research Group, said he suffered five hours of shaking chills, fever up to 101 degrees, severe headache, nausea, ringing in his ears and a sore arm after getting his booster dose of the Moderna vaccine. Poland explained that the second dose is amplifying the lessons of the first dose, which taught your body how to recognize the coronavirus as an enemy. “We should stress it doesn’t mean that anything’s going wrong or that something bad is happening. It is an expected reaction to the vaccine, and it will be different between different people. It is evidence of a vigorous immune response, which doesn’t mean that people who have less of a response are not developing an immune response. They are,” Poland added. “But for some of us, for whatever reason, our immune system sees this and really reacts to it” Poland said [5].
According to the U.S. Food and Drug Administration, both Moderna and Pfizer noted a more intense reaction to the second dose in their volunteers. Moderna specifically noted that “Grade 3” side effects swelling, pain, body aches, headache and fever were more frequently reported after the second dose than the first [6]. Now that we understand how the vaccine works and how it can potentially affect us, lets discuss ways to mitigate some of the symptoms and reactions associated with the Covid-19 vaccines.
Foods That Will Sooth Symptoms
According to the World Health Organization (WHO), the immune system requires the support of many nutrients. It is recommended to consume a variety of foods for a healthy and balanced diet, including whole grains, legumes, vegetables, fruits, nuts, and animal source foods [7]. There is no food that will stop anyone from catching Covid-19. There are, however, some foods that have been known to help one feel better after getting the second vaccine. Inflammation is one of the main culprits when it comes to the kind of discomfort one feels after the Covid-19 vaccines. According to verywellhealth.com, “inflammation is the immune system’s natural response to injury or illness. When you are injured or become sick, your white blood cells release inflammatory chemicals into the blood and affected tissues to protect the body from foreign invaders, such as bacteria and viruses [8]. Based on this information, after the vaccine is administered, the body goes into “fight” mode as something foreign has been introduced. There are foods that help to diminish inflammation and in turn, can make you feel much better.
Blueberries
Blueberries are an excellent source of antioxidants and while they can also sooth your sweet tooth, they also fight inflammation. Adding these to your unsweetened yogurt makes for a snack that will not only change your mood as they are known to also increase serotonin which is the hormone that balances your mood. The decrease in inflammation will help to make you feel much better after your vaccine [9,10].
Bone Broth
Bone broths and clear soups have plenty of nutrients and have been known to have major soothing effects. Because of this, bone broths will most certainly will make you feel better after your second Covid-19 vaccine. Consumer Health Digest tells us that bone broths help improve joint health due to the increased level of collagen it contains and gives the immune system a boost. Inedible animal parts such as bones and marrows along with tendons, ligaments, skin, and feet of beef, chicken, lamb, fish, and pork are boiled then simmered with fresh vegetables for an extended period. The result is a broth that is rich in nutrients and flavor and is easily digestible [11].
According to WebMD, A clear broth is warm and soothing, making it a great source of hydration while you are sick. Broths made with chicken are also high in tryptophan, which causes your body to produce serotonin, a mood enhancer and give you the feeling of comfort [12]. Jada Murray, a registered and licensed dietitian and instructor at Jacksonville State University in Jacksonville, Alabama states that “broths that are made with vegetables like carrots, onions and celery have vitamin K and vitamin C, and other minerals and antioxidants. These helps decrease inflammation, relax your muscles, and soothe the discomforts of cold or flu like symptoms, as well as build up a person’s immune system to help fight off viruses and help your body recover from illness more quickly [13].
Green Tea
Green tea is known as a superfood that offers an array of benefits. As one of the healthiest beverages on the planet, its most prevalent benefit is that is overflowing with polyphenol antioxidants that are known to reduce inflammation in the body. This is the very reason why green tea is a good bet for making your second Covid-19 vaccine easier to manage. According to Health.com these antioxidants proactively protect cells from damage which makes it a superfood that offers a wide range of health protections and benefits. Green tea antioxidants also offer antibacterial, antifungal, and antiviral effects that support immunity [14].
Turmeric
Turmeric is another superfood that can go a long way to ease the symptoms of the Covid-19 vaccinations. Curcuma longa better known as Turmeric, is a spice used for cooking, however, it has gained enormous popularity as one of a handful of powerful herbs for fighting various diseases. According to News-Medical. net, Betsaida B. Laguipo, a nutritionist who discusses the health benefits of turmeric, states that “turmeric contains more than 100 chemical compounds that contribute to its healing abilities. The best-known health benefit of turmeric is its anti-inflammatory and antioxidant properties, giving it the power to alleviate swelling and pain. Inflammation is a very common cause of pain and discomfort” [15]. The National Library of Medicine-National Institutes of Health says that turmeric “has been shown to be one of the best foods to maintain, protect, and boost immunity, reducing the risk of falling ill. It also has antiviral, antibacterial, and antimicrobial properties and can be used for pain relief. The curcumin that is found in turmeric is a potent antioxidant that can help neutralize free radicals and boost the activity of antioxidant enzymes in the body [16]. It can be added to tea, smoothies, soups, and salads.
Salmon, particularly wild caught salmon has lots of properties that can assist you in feeling better after your Covid-19 vaccines. While salmon is a great source of protein and Vitamin B as well as others, it also is one of the best sources of the long-chain omega-3 fatty acids EPA and DHA. Farm raised salmon is also a good source of these acids, but wild salmon contains at least 0.3 additional grams. Omega-3 fats can only be received via your diet as the human body cannot create them. Salmon as well as other fatty fish can help lower inflammation significantly, which helps to curtail risk factors for a few diseases and boost recovery in people with inflammatory conditions [17].
Green Vegetables
Another reason to eat your green vegetables is because the antioxidants in them could make your recovery from the Covid-19 vaccines much easier. Making sure we eat our vegetables is something parents have been preaching for decades, but with good reason. According to Jada Murray, a registered and licensed dietitian and instructor at Jacksonville State University in Jacksonville, Alabama, green vegetables (such as kale, broccoli, collards, and spinach) have high levels of antioxidants that help greatly to fight bodily inflammation. An antioxidant called sulforaphane, which is found in broccoli, helps to combat inflammation. Green vegetables are tremendous sources of beta-carotene, vitamin A, vitamin C, vitamin K, magnesium, potassium, as well as a host of other vitamins that are helpful. Ms. Murray also added that green leafy vegetables help your body in various ways such as boosting immunity, preventing infections, weight control and others.
Conclusion
While quite a few people experience no side effects from the Covid-19 vaccine, there are those that have reported some reactions like fatigue, aches, headaches, chills, and some even report fevers. The CDC says that that “you may have some side effects, which are normal signs that your body is building protection. These side effects may affect your ability to do daily activities, but they should go away in a few days [18]. Based on the information we have, the best way to get through the vaccine side effects will be to soothe the inflammatory immune response by focusing on foods that eliminate inflammation.
To read more about this article: https://irispublishers.com/gjnfs/fulltext/covid-vaccination-side-effects-and-foods-that-can-help.ID.000563.php
For more Open Access Journals in Iris publishers please click on: https://irispublishers.com/pdf/peer-review-process-iris-publishers.pdf
Wednesday, 2 June 2021
Iris publishers-Global Journal of Nutrition & Food Science (GJNFS)
A Double Hit: COVID-19 and Childhood Obesity
Authored by Courtney N Haun*
Introduction
It is evident that childhood obesity is a significant public health issue that is associated with various health morbidities [1]. Globally speaking, as of 2019, it was estimated that 38.2 million children under the age of 5 years were overweight or obese (World Health Organization, 2020). Additionally, over 340 million children and adolescents aged 5-19 were overweight or obese in 2016 (World Health Organization, 2020). Adding to this issue are the implications of the COVID-19 pandemic on children’s physical activity and nutrition across the world. Childhood obesity and COVID-19 is a “double hit” on adolescents’ health and their learning outcomes, exacerbating the issue of obesity even further.
Background
A prior study by Haun, et al. (2017) [2] revealed how school health programs and parental knowledge on health and nutritional issues plays a role in children’s health outcomes. Within many school systems, there are clear policies surrounding adequate physical activity and nutritional guidelines. However, due to COVID-19, many school systems chose to move to an online format to mitigate health risks from the virus. Parents and guardians were then tasked to accommodate these changes, where many children began learning primarily from home and outside of the school system [3]. Studies are already showing the negative effects this change is having on childhood obesity rates [4]. With the lack of physical education in the school system and stay-at-home orders, many children have experienced physical activity decline and weight gain.
Discussion
Now, while school systems are tittering between the in-person and online learning format, health interventions are urgently needed to help promote children’s physical activity at home. Recommendation from Rundle, et al. (2020) [5] suggest that there is a need for innovative approaches to address food insecurity within environments where children will continue to learn from home. The authors also recommend that school systems should build on their remote teaching capacity by making physical education a priority. The COVID-19 pandemic has also highlighted the need to timely, comprehensive healthcare for children and their families [6]. Solutions are still being explored and how the long-term effects from the interruption of children’s daily routine from in-person learning to online learning.
Conclusion
School health programs have a responsibility to promote environments where children are receiving adequate nutrition and physical activity, whether that is within the school walls or in the student’s homes. Childhood obesity and COVID-19 are both international pandemics, otherwise creating an increased risk for children to develop obesity. Parents and guardians now bear part of the responsibility to ensure a healthy environment for their children. Educators, healthcare providers, and communities must work to reduce the negative impact of obesity and COVID-19 with effective solutions.
To read more about this article: https://irispublishers.com/gjnfs/fulltext/a-double-hit-covid-and-childhood-obesity.ID.000562.php
For more Open Access Journals in Iris publishers please click on: https://irispublishers.com/pdf/peer-review-process-iris-publishers.pdf
Iris publishers-Global Journal of Nutrition & Food Science (GJNFS)| Wishing you a Happy Thanksgiving Day
Wishing you a Happy Thanksgiving Day

-
State of Food vs Income-Expenditure Gap in Developing World with a Focus on Iran Authored by Andrew J Rosenthal* The paper explores how in...
-
Global Journal of Nutrition & Food Science Effect of two simple drying methods (sun drying and oven drying at 40 °C, 50 °C and 60...
-
Iris Publishers-Quora Welcome to IRIS Publishers , your one-stop-place for latest scientific! Here you can read from our vast archi...





